PHS is rolling out the Lifeguard overdose alert app in our supportive housing and shelters in Vancouver and Victoria.
We work hard to provide ways for our community to use safety. We offer many different kinds of opportunities for witnessed consumption so there’s someone on hand to administer the overdose-reversing drug naloxone, if needed. Lifeguard is aimed at those who, for whatever reason, are not using in those observed spaces. It’s a safety device for those using alone.
Opioids depress breathing, which becomes increasingly shallow and irregular, whilst also causing sedation. In an overdose, it’s the lack of oxygen that proves fatal. And it’s impossible for an individual slipping into unconsciousness to self-administer naloxone.
This is where the Lifeguard Digital Health app comes in.
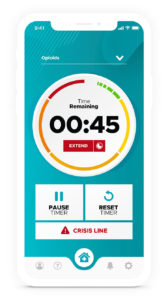
It’s a simple concept, based around a timer. Someone ready to consume drugs sets an alarm, which gives them 50 seconds until an alert sounds. If they are not responsive enough to pause or stop the alarm, an emergency call goes out to paramedics and PHS staff nearby.
Although the technology raises the alarm; the opioid poisoning is still responded to in person with naloxone and, most likely, bottled oxygen.
PHS received a grant through Health Canada’s Substance Use and Addictions Program (SUAP) in July, enabling us to provide the Lifeguard app throughout all our supportive housing and shelters. It’s a system-wide pilot program based on an earlier trial which showed two things: residents used the app, and it successfully raised the alarm if they overdosed.
 As the program rolls out, residents’ rooms are being fitted with a proprietary device that resembles a cross between a tablet and a smartphone, but does only one thing. It operates the Lifeguard app.
As the program rolls out, residents’ rooms are being fitted with a proprietary device that resembles a cross between a tablet and a smartphone, but does only one thing. It operates the Lifeguard app.
“People always have reasons for wanting to use alone,” said PHS Senior Housing Manager Duncan Higgon. “And all the naloxone and oxygen in the world is meaningless to me if I don’t know if someone is using in their room.
“Some people use alone because of their feelings of stigma. Probably the person who feels this the most is the person going through recovery. Their identity is shaped around not using, and they keep it secret.
“There are other reasons people don’t want to be seen taking drugs. If you think about it, if I owe you $60 but I’ve got $30 of dope, I can’t use that in front of you.
“Or maybe it’s someone in a relationship, and they have just enough to avoid being dope sick, but there’s an expectation they would share.”
There is no one-size-fits-all solution to the drug poisoning crisis. It’s a multi-faceted emergency that challenges us to keep bringing forward new ideas and trying novel approaches.
Lifeguard is one of our new approaches.
- Learn more about innovative PHS programs and our supportive housing in Vancouver and Victoria, B.C.
- Donate to continue innovative projects like these.



